HCCs are increasingly used as a way to risk-adjust patients in multiple VBR programs. For example, CMS HCCs are used as a factor in calculating the total performance score (TPS) under the Hospital Value-Based Purchasing (VBP) Program, and they are often used in shared risk and shared savings program metrics.
HCC & Risk Adjustment Factor
- HCC (Hierarchical Condition Categories) is a model implemented to adjust capitation payments to private healthcare plans for the health expenditure risk of their enrollees
- The CMS risk adjustment model measures the disease burden that includes 79 HCC categories, which are correlated to diagnosis codes
- The HCC model is made up of 10,000+ ICD-10 codes that typically represent costly, chronic diseases such as:
- Diabetes
- Chronic kidney disease
- Congestive heart failure
- Chronic obstructive pulmonary disease
- Malignant neoplasms
- Some acute conditions (MI, CVA, hip fx)
Risk Score Development
The Risk Adjustment Factor (RAF score) is set for each patient and includes:
- Baseline demographic elements (age/sex, dual eligibility status).
- Incremental increases based on HCC diagnoses submitted on claims from face to face encounters with qualified practitioners during the calendar year.
- HCC coding is prospective in nature - the work you do in this year sets the RAF and subsequent funding for next year.
- All models include chronic conditions that do not change from year to year, i.e., diabetes, COPD, CHF, Atrial-Fib, MS, Parkinson’s, Chronic Hepatitis.
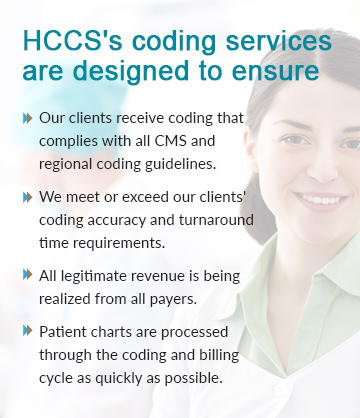
Coding Team Midas IT Services
- Our fully-employed team of certified coders can scale quickly and complete projects of any size with the maximum level of accuracy, and following a rigorous quality assurance process.
- CPC/CRC Certified coders to perform chart review to identify all HCC conditions.
- Coders are well versed with CMM HCC specifications and ICD-10 CM coding guidelines .
- Certified physician auditors to ensure 98% accuracy.
- AHIMA approved ICD-10 coding trainers.
Chart Review
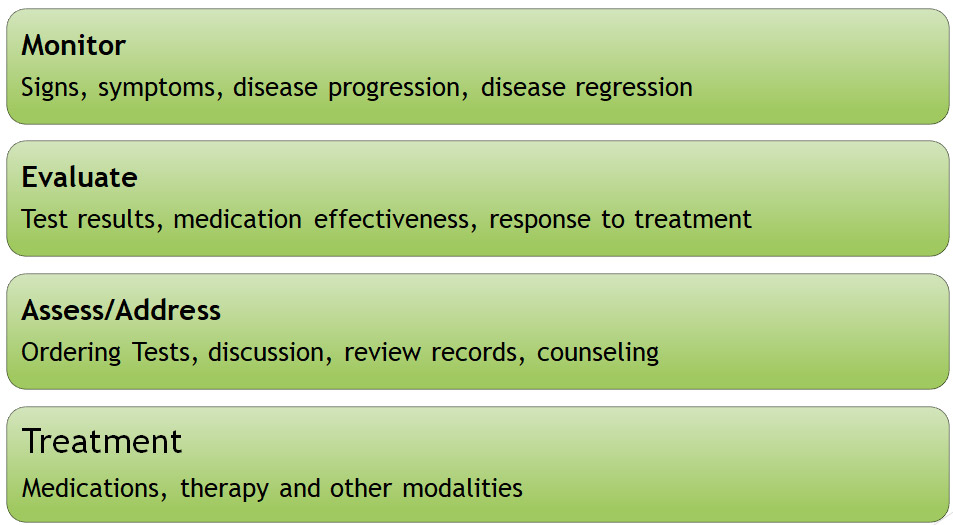
- Capturing of all HCC codes with assigned HCC condition category, Documentation must show that condition was monitored, evaluated, assessed, or treated (MEAT).
- Follow ICD-10 Official Guidelines for Coding and Reporting. Adherence to these guidelines is required under HIPAA.
- Coding of all ICD-10 CM codes mapped to 79 HCC categories.
- Review of complete medical record, not only from problem list or PMH.
- Identification of conditions which are not documented but billed.
MEAT for HCC conditions
Risk Adjustment Calculation
- Individual risk scores are calculated by adding the coefficients associated with each members demographic and disease factors.
- RAF calculation at the member and practice/plan level.
- RAF improvement for each member (Last year base RAF score to be shared by client).
HCC Reporting
- Average HCC per member within reviewed population.
- Top 10 HCC conditions, raw data also can be shared based on client requirements.
- Top 10 HCC conditions with higher RAF value.
- Identification of Undocumented HCC conditions to eliminate coding compliance risks.
- Weekly/monthly project review to share progress.
- Project end summary with complete output details.
Output Files Submission
- HCC output files submission in standard file format or client preferred format if any.
- 100% quality audit on output files to reduce any data discrepancy.
- Secure data files sharing via SFTP or encrypted files.
 business@midaswebtech.com
business@midaswebtech.com